What Makes Sydney’s Tattoo Culture So Unique in 2024?
Sydney tattoo culture 2024 stands as one of the most dynamic and diverse body art scenes globally. The city has transformed from viewing tattoos as rebellious statements to embracing them as legitimate art forms worthy of galleries and museums.
The evolution traces back decades, with waves of cultural influence shaping today’s landscape. Pacific Islander traditions brought bold tribal patterns, Japanese immigrants introduced intricate Irezumi techniques, and European settlers contributed old-school American styles. This multicultural foundation created a melting pot where artists freely blend techniques and philosophies.
Tattoos serve as visual autobiographies for Sydneysiders. Each piece tells a story—commemorating lost loved ones, celebrating personal milestones, or expressing core values. Walk through Newtown or Bondi, and you’ll witness this narrative diversity: a software developer sporting delicate line work, a chef wearing full Japanese sleeves, a teacher with subtle geometric patterns.
The Sydney Best Tattoo Designs: The 5 Most Requested Styles This Year showcase this cultural richness. Studios across Surry Hills, Darlinghurst, and Bondi Beach push creative boundaries while respecting traditional techniques. Artists collaborate with clients to craft custom pieces that honor both timeless artistry and contemporary innovation.
This unique blend positions Sydney as a global tattoo destination where tradition meets cutting-edge creativity.
1. Why Are Freehand Tattoos Taking Over the Streets of Sydney?
Freehand tattoos Sydney artists are creating buzz by ditching stencils entirely and drawing directly onto skin. This technique transforms the body into a living canvas, where artists sketch and ink simultaneously, allowing designs to flow naturally with each person’s unique contours and movements.
The method demands exceptional skill and confidence from tattoo artists. They must visualize the complete design while adapting to the body’s natural curves, muscle definition, and bone structure. This spontaneous approach creates pieces that simply cannot be replicated—each tattoo becomes a singular work of art shaped by the moment of creation.
One of the key distinctions between freehand tattoos and traditional methods is highlighted in discussions about the difference between transfer vs freehand tattoos. While traditional tattoos often rely on stencils or transfers, freehand tattoos allow for a more personalized and organic approach.
Popular freehand designs include:
- Flowing botanical pieces that wrap organically around limbs
- Abstract patterns that respond to body movement
- Custom lettering that follows natural body lines
- Ornamental designs tailored to specific placement
Sydneysiders gravitate toward freehand tattoos because they reject cookie-cutter designs. The technique appeals to those who value authenticity and want their body art to feel genuinely personal. When an artist draws freehand, they consider your body’s unique architecture, creating something that exists nowhere else in the world.
The collaborative nature of freehand tattooing also resonates with Sydney’s creative community. Clients witness their tattoo’s birth in real-time, participating in an intimate artistic process that strengthens the connection between wearer and artwork.
2. Why Are Delicate Line Tattoos So Popular in Sydney?
Delicate line tattoos are popular among many people in Sydney because of their thin and precise designs that exude elegance. These minimalist tattoos are created using a single-needle technique, resulting in clean and delicate lines that sit softly on the skin without being overpowering.
The Versatility of Delicate Line Tattoos
One of the main reasons why these tattoos are so appealing is their versatility. They can be customized to suit individual preferences and can represent various meanings or symbols.
Some common themes found in delicate line tattoos include:
- Nature-inspired designs: Such as flowers, leaves, and other botanical elements
- Animal motifs: Including silhouettes of birds, cats, or marine creatures
- Geometric patterns: Incorporating shapes like triangles or circles
- Symbolic representations: Depicting meaningful icons or symbols
Who Is Attracted to Delicate Line Tattoos?
The appeal of delicate line tattoos extends to different age groups and backgrounds. Here are some examples of who may be drawn to this style:
- Professionals looking for discreet tattoos that can be easily covered up at work
- Individuals getting their first tattoo and wanting something subtle
- People who appreciate fine art and craftsmanship in tattooing
The Longevity and Placement Options
When done by skilled artists, delicate line tattoos have the potential to age well over time. The lines remain crisp and defined even after years have passed since getting inked.
Another advantage of these tattoos is their intimate size, which allows for placement in hidden areas such as wrists, behind ears, or along collarbones. This makes them an ideal choice for those who prefer keeping their body art private while still expressing themselves.
Social Media Influence
In recent years, social media platforms like Instagram have played a significant role in popularizing delicate line tattoos. Their visually appealing nature makes them highly shareable online, inspiring many Sydney residents to embrace this refined aesthetic.
The combination of all these factors contributes to the allure of delicate line tattoos among people in Sydney.

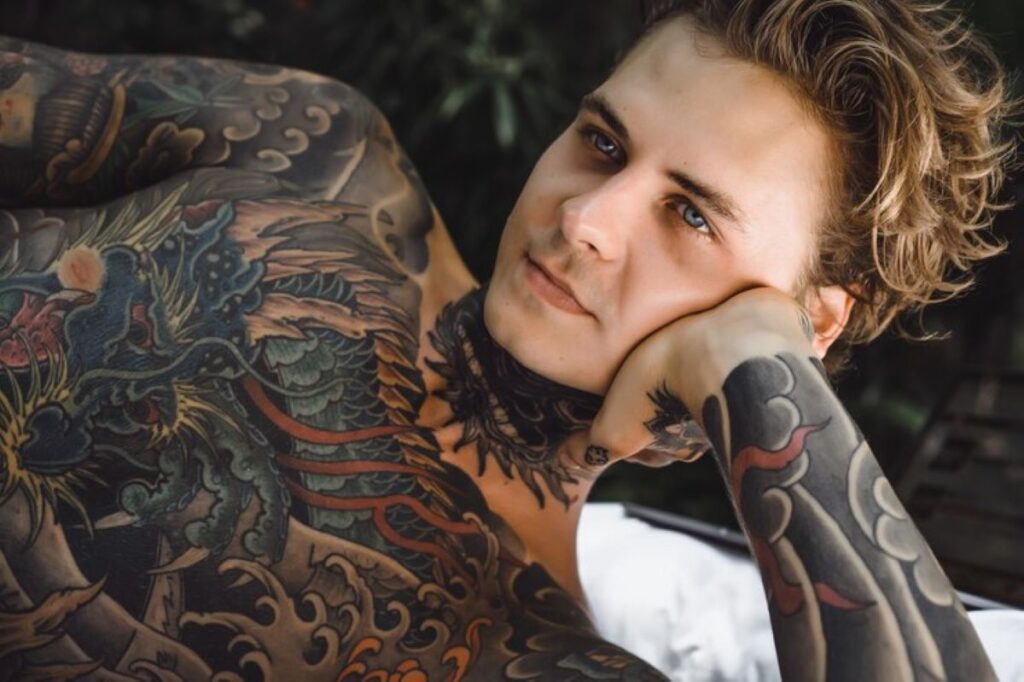
3. Why Do Japanese Tattoos Continue to Captivate Sydneysiders?
Japanese tattoos Sydney remain one of the most sought-after styles because they combine centuries-old tradition with deeply symbolic storytelling. Irezumi (or Horimono) represents more than decorative art—each element carries specific cultural meaning rooted in Japanese mythology, folklore, and spiritual beliefs.
The intricate imagery that defines these Japanese tattoos Sydney pieces includes:
- Samurai warriors symbolizing honor, courage, and unwavering loyalty
- Geisha women representing beauty, grace, and the refined arts
- Koi fish embodying perseverance, transformation, and overcoming adversity
- Dragons signifying wisdom, strength, and protection
- Cherry blossoms reflecting life’s fleeting nature and beauty
These designs demand exceptional technical skill. Artists must master traditional shading techniques, understand proper placement on the body’s contours, and respect the cultural significance behind each symbol. The bold color palettes—vibrant reds, deep blues, and rich blacks—create striking contrast that ages beautifully.
Authentink in Surry Hills stands as Sydney’s premier destination for authentic Japanese tattooing. Their artists have studied traditional methods and maintain the discipline required for these complex pieces. The studio’s commitment to cultural authenticity ensures clients receive genuine Irezumi work rather than superficial imitations.
These tattoos often require multiple sessions spanning months or years, particularly for full sleeves or back pieces. The investment reflects both the artistry involved and the permanent connection to Japanese cultural heritage.
4. Why Do Sydneysiders Love Realism Tattoos?
Realism tattoos Sydney artists create pieces that look exactly like photographs, capturing every shadow, texture, and subtle detail with stunning accuracy. These designs replicate the exact appearance of their subjects, whether human faces, animals, or objects, transforming skin into a living canvas of lifelike imagery.
The Emotional Connection
The emotional significance behind these tattoos drives their popularity. Many Sydneysiders choose portraits of family members, partners, or children as permanent tributes to their relationships. Pet portraits rank equally high, with dog and cat lovers immortalizing their companions in breathtaking detail. Some opt for spirit animals—wolves representing loyalty, eagles symbolizing freedom, or lions embodying strength—that reflect personal values and characteristics.
The Skill Behind the Art
Creating these masterpieces demands exceptional technical skill. Artists must understand:
- Light source direction and shadow placement
- Skin tone variations and color blending
- Depth perception through shading techniques
- Anatomical proportions and facial features such as in-depth understanding on how to illustrate heads, faces and facial features
- Aging considerations as skin changes over time
Studios like Lighthouse Tattoo and Hunter & Fox employ specialists who’ve spent years perfecting photorealistic techniques. The process typically requires multiple sessions, with artists working from high-resolution photographs to ensure accuracy. This meticulous approach explains why realism tattoos command premium pricing—clients aren’t just paying for ink, but for an artist’s mastery in translating three-dimensional reality onto a two-dimensional, curved surface that breathes and moves. Check out more about best fine line tattoo artists sydney: where to go for clean, ultra-precise detail.
Which Tattoo Studios Are Leading the Way in These Trending Styles?
Authentink in Surry Hills is Sydney’s top choice for traditional Japanese tattoos. Here, skilled artists use age-old Irezumi techniques, paying close attention to cultural accuracy and symbolic intricacies.
Lighthouse Tattoo in Botany has earned a reputation for its adaptability. The studio boasts a team proficient in various styles, including Japanese traditional and lifelike portraiture. Their personalized approach guarantees that every client receives a tattoo that perfectly aligns with their vision, regardless of their preferred style.
Bondi Ink gained international fame through its reality show, but the studio’s true success lies in its exceptional talent. The artists here effortlessly switch between different styles—ranging from intricate line work to striking realism—making it a popular choice for clients seeking a wide range of design options all in one place.
These best tattoo studios Sydney 2024 have something in common: they don’t just follow trends, they create them. Each studio upholds strict hygiene practices while nurturing an atmosphere where artistic creativity flourishes. Their artists consistently enhance their skills, participate in global conventions, and collaborate with clients to turn personal narratives into everlasting art.
Where Can You Find Your Dream Tattoo Design in Sydney?
Instagram and Pinterest are great platforms to find tattoo design inspiration. They have a wide range of galleries showcasing the work of top tattoo artists in Sydney. You can explore hashtags such as #SydneyTattoo or #SydneyBestTattooDesigns to discover popular styles and portfolios of artists. Make sure to save any designs that resonate with you, but keep in mind that these should only serve as ideas and not dictate your final piece. Customization is key in turning generic concepts into personal statements.
When looking for tattoo shops in Sydney, it’s important to research each studio’s portfolio to ensure they have expertise in your preferred style. Here are some factors to consider:
- Artist specializations: Check if the artists specialize in Japanese, realism, line work, or freehand techniques.
- Client reviews: Read reviews on Google and social media platforms to get an idea of the studio’s reputation.
- Hygiene certifications: Ensure that the studio maintains high cleanliness standards and has proper hygiene certifications.
- Consultation processes: Find out how the studio conducts consultations and if they prioritize understanding your vision.
Studios like Authentink are known for their exceptional Japanese designs, while Lighthouse Tattoo offers versatility across various techniques. It’s a good idea to book consultations with 2-3 artists to compare their approaches. The right artist will not only enhance your concept but also respect your original vision. Quality studios value collaboration and strive to create tattoos that tell your unique story instead of simply copying existing designs.
Embrace Your Individuality Through Tattoos
Embracing individuality through tattoos means choosing designs that genuinely represent your story, beliefs, and aesthetic preferences. Each of the Sydney Best Tattoo Designs: The 5 Most Requested Styles This Year offers distinct ways to express who you are—whether through the spontaneity of freehand work, the elegance of delicate lines, or the depth of Japanese symbolism.
Your tattoo becomes a permanent reflection of your journey. Take time browsing multiple artists’ portfolios to find someone whose vision aligns with yours. The right artist will understand your concept and translate it into meaningful body art that you’ll cherish for life.